If you’ve ever felt overwhelmed by the sheer number of birth control options out there, you’re not alone. With so many methods available—some common, some more unusual—it’s often difficult to make an informed decision that truly fits your body, your lifestyle, and your wellness goals. Whether hormones are a no‑go for you, whether you want something long‑term or more temporary, knowing the pros, cons, and efficacy of each method can make all the difference.
Let’s explore the major birth control methods, along with some lesser‑known but totally valid alternatives. We’ll compare hormonal vs non‑hormonal, natural vs medical, short‑term vs permanent, so you can feel confident about whatever path you choose. And yes, there are two methods that are 100% effective—the rest, while highly effective when used correctly, carry some risk.
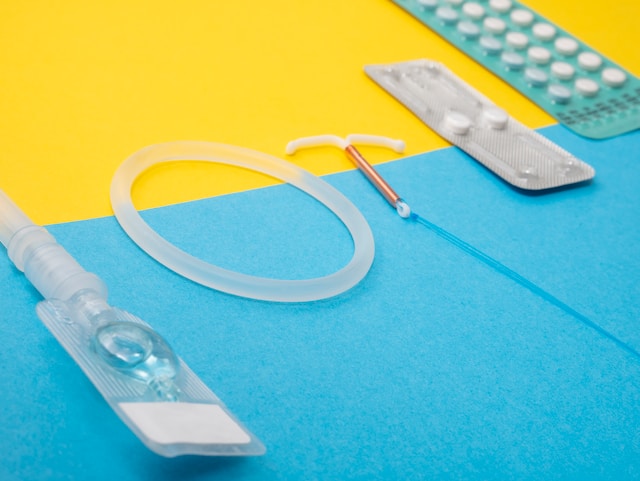
Most Common Birth Control Methods (and How They Actually Perform)
Here are the contraceptive methods most people are familiar with. All are used by millions, most with very high efficacy—when used exactly as directed.
IUDs (Intrauterine Devices)
One of the top birth control methods in terms of reliability and user satisfaction. An IUD is a small, T‑shaped device placed into the uterus. You can choose a hormonal IUD (releasing progestin) or a copper IUD (non‑hormonal). Each prevents pregnancy by making it hard for sperm to reach the egg, and for fertilization to happen.
-
Efficacy: Over 99% effective.
-
Biggest advantages: Once in, pretty much forget about it until you’re ready to conceive—your practitioner can remove it. Some IUDs last 3‑10 years depending on type.
-
Drawbacks: No protection against STIs. Hormonal IUDs may cause hormonal side effects (spotting, irregular bleeding, mood shifts). Copper IUDs can sometimes cause heavier or more painful periods. Also: both the insertion and the removal of an IUD is very painful and if you are prone to vaginal infections, IUDs may increase the number of infections you have.
Hormonal vs Barrier vs Natural Contraception
Before going into more methods, it helps to understand the difference between hormonal contraception (implants, pills, shots, rings, hormonal IUDs), non‑hormonal barrier methods (condoms, diaphragms, caps, sponges, copper IUD), and natural contraception or fertility awareness methods. Each category has different trade‑offs in terms of side effects, convenience, cost, and how effective it is in real life (which is usually lower than the perfect‑use lab numbers due to missed doses, improper use, etc.).
Condoms (Barrier method)
Condoms are probably the most well‑known non‑hormonal contraception. Latex, synthetic, or natural (lambskin) versions are available. With male condoms, you block sperm from entering the uterus. Female condoms also exist, but are less popular.
-
Efficacy: About 87% typical use.
-
Pros: No hormones, plus many protect against STIs (especially latex or synthetic). Good for occasional or shared use.
-
Cons: Must be used each time correctly. They can break or slip. Some people find they interrupt spontaneity or “the mood,” though many others make it part of the experience.
Birth Control Implant
This is a small rod inserted under the skin (usually in your arm) that releases progestin continuously. It prevents ovulation and thickens cervical mucus so sperm can’t reach the egg.
-
Efficacy: Around 99%, over multiple years (often 3‑5 years depending on the implant).
-
Pros: Set‑and‑forget convenience; high reliability.
-
Cons: Hormonal side effects such as mood changes, bleeding irregularities; once inserted, requires medical removal if you change your mind; possible weight changes or impact on menstrual patterns.
Shot, Ring, Patch (Short‑acting Hormonal Methods)
These are hormonal options that require regular attention: a shot every few months, a vaginal ring (monthly), or a patch you replace weekly.
-
Efficacy: Usually in the 93‑96% range with perfect use; somewhat lower with typical use.
-
Pros: Flexible choices; less frequent maintenance (especially with the shot or ring).
-
Cons: Introduce synthetic hormones, which can lead to side effects (headache, nausea, breast tenderness, mood swings, maybe increased clot risk). If you miss changing ring or patch on schedule or delay shot, the risk increases.
The Birth Control Pill
The daily pill remains one of the most common hormonal birth control methods. You take it every day at roughly the same time; it works by suppressing ovulation and affecting cervical mucus and uterine lining.
-
Efficacy: When used perfectly, ~99%; typical use brings that down to about 93%.
-
Pros: Widely available; many different formulations so you might find one that fits your body; can help with menstrual regulation, acne, mood issues for some. Often covered by insurance.
-
Cons: Daily commitment. Possible side effects like mood swings, weight gain, nausea, increased risk (especially for smokers over 35) of certain issues (blood clots, etc.). Also, after stopping, fertility may take a bit to bounce back for some people.
Emergency Contraception (Plan B / Morning‑After Pill)
Used after unprotected sex or contraceptive failure (e.g. condom broke) to prevent pregnancy. Should be taken as soon as possible.
-
Efficacy: Decreases the longer you wait; best within 24 hours, still can work up to about 72 hours (and sometimes longer depending on formulation).
-
Pros: A one‑time solution, gives a “backup” when something slips.
-
Cons: Not for routine use; potential side effects (nausea, fatigue, disruption of next period). Decreased effectiveness with time.
Less Common Methods: Natural, Barrier, and Permanent Options
If you’re looking for non‑hormonal or more sustainable, permanent, or natural birth control methods, these options might appeal.
Diaphragms & Cervical Caps
These are barrier methods you insert into the vagina to block the cervix. Diaphragms usually are used with spermicide; cervical caps may be too.
-
Pros: Hormone‑free; little systemic side effects; can be used only when needed (not continuous).
-
Cons: Must be inserted properly; risk of irritation or infection; somewhat lower efficacy vs hormonal/long‑acting methods; spermicide can irritate some people.
Sponges & Spermicide Alone
Sponges soaked with spermicide or spermicide on its own acts to kill or block sperm.
-
Pros: Hormone‑free, over‑the‑counter; used only as needed.
-
Cons: Among the less effective methods if used typically—rates like 70‑80% with typical use; possible risks of irritation; less predictable.
Fertility Awareness / “Rhythm Method” / Natural Family Planning
These methods involve tracking your menstrual cycle, basal body temperature, cervical mucus, sometimes using apps or ovulation predictor kits. Recognizing when you are most fertile and avoiding intercourse (or using barrier/hormonal backup) during that window.
-
Pros: No hormones; helps you understand your body and cycle; low cost (just apps, possibly basal thermometers, time). Many people find that knowing their cycle helps with health awareness beyond just pregnancy prevention.
-
Cons: Requires diligence, consistency, daily tracking; less reliable if you have irregular cycles; easy to make mistakes; does not offer STI protection.
Permanent Solutions: Sterilization
For people who are certain they do not want future pregnancies, sterilization offers a permanent option. Common procedures include:
-
Vasectomy (for men): surgical procedure to cut or seal the tubes that carry sperm.
-
Tubal ligation or tubal occlusion (for women): surgical closure or removal of fallopian tubes.
-
Efficacy: Very close to 99%; effectively lifelong.
-
Pros: Once done, no need to worry about birth control again (except guarding against STIs separately).
-
Cons: Surgery—costs, recovery time, possible risks; generally irreversible (or very challenging to reverse). Could have regret for some people.
Comparing Efficacy & Considering What Matters Most
When choosing, here are a few things to think through:
-
Efficacy in real life vs perfect use: Methods like IUDs and implants have very high effectiveness even with typical use, because once in place you don’t have to remember anything. Pills, patches, rings, fertility awareness have more “user burden,” so mistakes or missed doses reduce effectiveness.
-
Hormonal vs non‑hormonal: Some people prefer to avoid synthetic hormones due to side effects like mood changes, weight change, nausea, or longer‑term concerns. Non‑hormonal methods (copper IUD, condoms, barrier methods, natural methods) tend to have fewer hormonal effects but may have trade‑offs in terms of effectiveness or convenience.
-
Protection against STIs: Only barrier methods (like condoms, diaphragms to some extent) reliably protect against STIs. Almost all hormonal or internal methods do not.
-
Side effects & impact on your menstrual cycle: Things like irregular bleeding, heavier or lighter periods, or loss of periods (amenorrhea) are real possibilities. Some women love that; some find it scary or unsettling.
-
How long you want it: Are you looking for something temporary (a few months or a year) or more long‑term (5+ years) or even permanent? That will change what methods make sense.
-
Cost, access, ease of use, comfort: Whether you have to pay out‑of‑pocket, whether your health plan covers it, whether you have to visit a doctor frequently, whether you’re comfortable with insertion/removal, etc.
The Two “Foolproof” Methods
Just to be totally clear, the only two methods that are actually 100% effective: abstinence (not having vaginal intercourse) and outercourse (sexual activity without penetrative sex). If those are in your toolbox, they’re totally effective—but of course, not always what people want or are in situations to use.
Making Your Decision
If I were you, I’d start by asking yourself a few questions:
-
What are your priorities? (Maximum pregnancy prevention? Avoiding hormones? No daily routine? Reversible methods? STI protection?)
-
How do you feel about introducing synthetic hormones into your body?
-
How regular is your cycle? Do you mind tracking every day?
-
How soon might you want to try for pregnancy? (Is this short‑term or longer‑term contraception?)
-
What side effects are you willing (or unwilling) to tolerate?
-
What is your budget / what does your insurance cover? Then, talk with a healthcare provider—ideally someone who listens and gives you all the options. And don’t be afraid to change your mind. What suits you now may not suit you in a few years, and that’s okay.
Balance, Awareness, & Informed Choice
Birth control is deeply personal. What works best for your body, hormones, wellness, emotional health, and life stage might not be what someone else chooses. Beware of “set it and forget it” advice without weighing side effects or non‑hormonal methods. Also beware of any myths—there’s a lot of misinformation out there about infertility, “natural” vs “artificial,” what hormones really do.
You deserve a birth control method that respects your body and your values, one that you feel comfortable with, that works well for your lifestyle, and gives you the efficacy and protection you need. Research, ask questions, give yourself permission to change paths if needed. With the right information, you can find a method that feels just right—empowering, respectful, and aligned with your wellness journey.